UC research focuses on key protein in heart failure
Study results will identify potential therapeutic targets
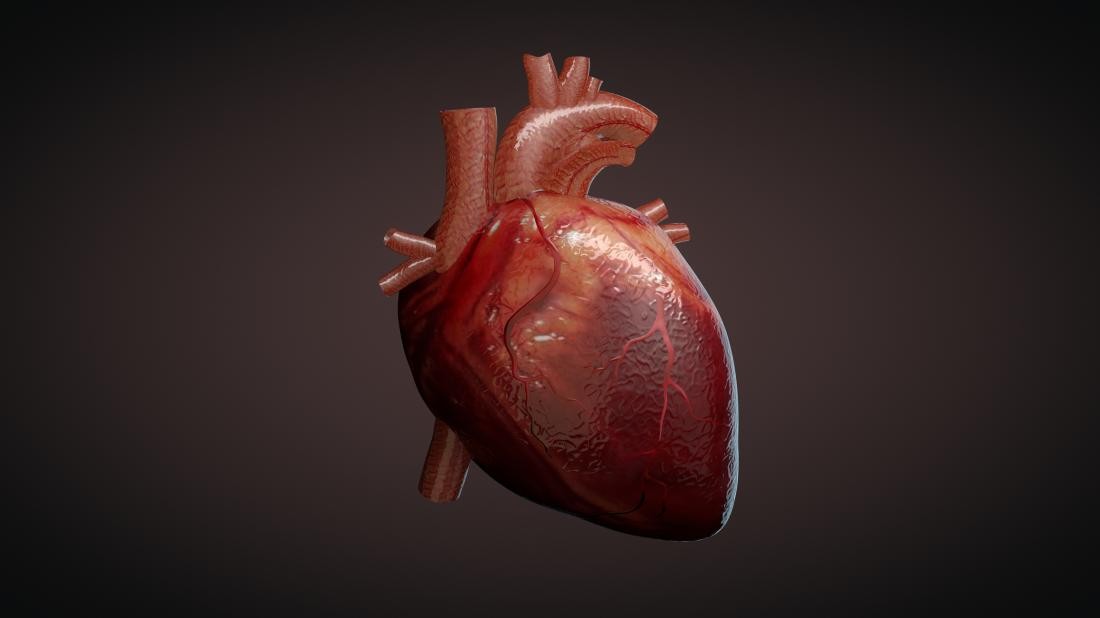
Research from the University of Cincinnati is examining a protein that plays a key role in heart failure.
The study is funded by the National Heart, Lung, and Blood Institute for just over $2 million dollars for four years and is a second renewal of a previous grant given to Sakthivel Sadayappan, PhD, professor in the Division of Cardiovascular Health and Disease in the Department of Internal Medicine at the UC College of Medicine.
Heart disease is a complex clinical syndrome that is a predominant cause of mortality in adults, says Sadayappan. With all the technology and treatment options, heart disease is still the number one killer worldwide and the leading cause of death for men and women in the U.S.

Sakthivel Sadayappan, PhD, professor in the Division of Cardiovascular Health and Disease in the Department of Internal Medicine at the UC College of Medicine/Photo/Colleen Kelley/UC Creative + Brand
The month of February has been designated as American Heart Month, which is dedicated to focusing on heart health. Over several decades, Sadayappan and his research lab have focused on understanding the exact causes, signals and defects that cause heart disease so that it can be either prevented or cured. In the current project, he and his team study the impact of the appearance of skeletal muscle protein in the heart during heart disease.
“In our preliminary study, we discovered that the protein is expressed or being used in the failing animal hearts and biopsies from heart failure patients,” says Sadayappan, the principal investigator for the study. “So, the question we asked was, ‘What is the skeletal muscle-specific protein expressed in the heart? What is its role in the heart? Is it helping the condition of heart failure or is it bad for treating heart failure?’”
The long-term objective of the research is to understand the functional consequences of the family of proteins on heart function in health and heart failure, according to Sadayappan. The research uses animal models to express the protein in the heart, which Sadayappan says is functionally beneficial, but not for the whole organ. Instead, that causes pain in the organ.
“This funding will determine why and how this phenomenon occurs,” says Sadayappan. “We don’t know that now. If it turns out that this process is beneficial, then we can use it as a gene therapy. We can use therapy on heart failure patients, and then see if we can improve their cardiac function. Or if it’s bad, we can use gene therapy to remove the protein in heart failure patients, and then that can be beneficial.”
Evangelia “Litsa” Kranias, PhD, Hanna Professor of Pharmacology and Systems Physiology, Distinguished University Research Professor, serves as a co-investigator in the study.
Next Lives Here
The University of Cincinnati is classified as a Research 1 institution by the Carnegie Commission and is ranked in the National Science Foundation's Top-35 public research universities. UC's medical, graduate and undergraduate students and faculty investigate problems and innovate solutions with real-world impact. Next Lives Here.
Related Stories
Sugar overload killing hearts
November 10, 2025
Two in five people will be told they have diabetes during their lifetime. And people who have diabetes are twice as likely to develop heart disease. One of the deadliest dangers? Diabetic cardiomyopathy. But groundbreaking University of Cincinnati research hopes to stop and even reverse the damage before it’s too late.
App turns smartwatch into detector of structural heart disease
November 10, 2025
An app that uses an AI model to read a single-lead ECG from a smartwatch can detect structural heart disease, researchers reported at the 2025 Scientific Sessions of the American Heart Association. Although the technology requires further validation, researchers said it could help improve the identification of patients with heart failure, valvular conditions and left ventricular hypertrophy before they become symptomatic, which could improve the prognosis for people with these conditions.
Combination immunotherapy helps overcome melanoma treatment resistance
November 10, 2025
MSN highlighted research led by the University of Cincinnati Cancer Center's Trisha Wise-Draper showing a combination of immunotherapy medications can activate a robust immune response and help overcome treatment resistance in patients with refractory melanoma.
