UC researchers use tech to help people with speech impediments
For many, talking comes so naturally that we rarely think about it. But there’s a lot at play when we talk: our lips, teeth and tongues all work together to produce desired sounds. Even our nose plays a part in this routine – pronouncing “n” or “m” rely on coordination between the mouth and nose.
People affected by a structural disorder called velopharyngeal insufficiency (VPI), however, have difficulty properly pronouncing sounds that are supposed to bypass the nose. Researchers at the University of Cincinnati are exploring the effects of VPI in an effort to inform potential treatments. The work is part of a five-year grant awarded by the National Institutes of Health.
This research is some of the first of its kind and reflects UC’s innovative agenda and strategic direction, Next Lives Here.
“We’re trying to tell surgeons what’s going on that affects these people’s speech,” says UC biomedical engineering Ph.D. candidate Michael Rollins. “If surgeons don’t know what’s making that sound in their speaking, then it’s tough to fix it.”
Rollins’ presentation of the team’s work was recently awarded second place in the student poster competition at the Acoustical Society of America meeting in Victoria, British Columbia.
We’re trying to tell surgeons what’s going on that affects these people’s speech.
Michael Rollins, UC Ph.D. candidate
People with VPI have an irregularity between their nose and mouth that affects certain sounds, Rollins explains. As the people send air into their nasal passage to speak, the resulting speech is distorted. There are three hypothesized sound sources that cause the distortion: mucous bubbling, aerodynamic turbulence and fluttering tissue.
“Depending on what’s making the sound distortion is going to inform how you treat it,” says Rollins.
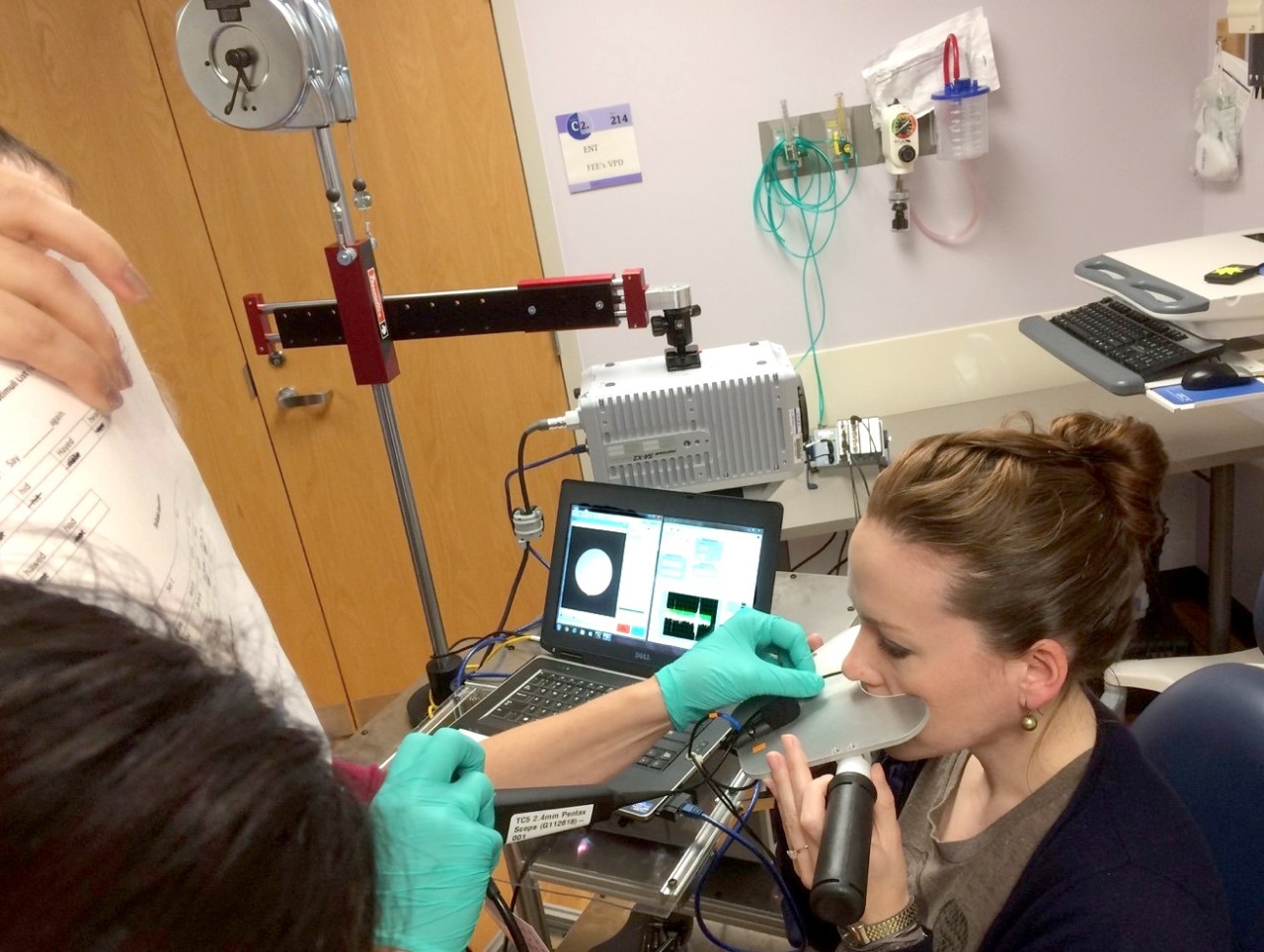
Rollins and the UC team observed ten patients from the VPI clinic at Cincinnati Children’s Hospital using a high-speed video camera and two microphones – one at the nose and one at the mouth. The researchers inserted the camera through the nose and recorded movement, such as from tissue displacement and mucus, in the nasal passage.
Pairing this video with the audio segments, the team determined that most of the patients were affected by mucous bubbling, also known as nasal rustle. In other words, when the patients inadvertently sent airflow to their nose to speak, the mucus in the nasal passage was fluttering, distorting the speech.
“What we saw was that while there’s not much mucus there, it’s dancing in the breeze,” says Rollins. One of the research team members lightheartedly refers to the motion as a “snot ballet.”
If mucus is the underlying cause, says Rollins, surgery may not even be necessary. Rather, blowing your nose or taking an allergy medicine may do the trick.
Rollins is in the process of preparing a manuscript to publish the findings in a journal. After that, he and the team will turn their attention to testing other sound sources that may cause VPI, like aerodynamic turbulence.
For those it affects, VPI has significant impacts on daily lives. With the research being done at UC, clinicians may finally have the data needed to correctly tackle this issue.
Featured image at top: A researcher demonstrates the equipment on an adult. The endoscope enters through the nose and views the oral-nasal passage from above, transmitting a live video of the motion to the computer. Microphones separated by a metal plate record the sound coming out of the nose and the mouth.
Next Lives Here
The University of Cincinnati is classified as a Research 1 institution by the Carnegie Commission and is ranked in the National Science Foundation's Top-35 public research universities. UC's graduate students and faculty investigate problems and innovate solutions with real-world impact. Next Lives Here.
Related Stories
Sugar overload killing hearts
November 10, 2025
Two in five people will be told they have diabetes during their lifetime. And people who have diabetes are twice as likely to develop heart disease. One of the deadliest dangers? Diabetic cardiomyopathy. But groundbreaking University of Cincinnati research hopes to stop and even reverse the damage before it’s too late.
App turns smartwatch into detector of structural heart disease
November 10, 2025
An app that uses an AI model to read a single-lead ECG from a smartwatch can detect structural heart disease, researchers reported at the 2025 Scientific Sessions of the American Heart Association. Although the technology requires further validation, researchers said it could help improve the identification of patients with heart failure, valvular conditions and left ventricular hypertrophy before they become symptomatic, which could improve the prognosis for people with these conditions.
Combination immunotherapy helps overcome melanoma treatment resistance
November 10, 2025
MSN highlighted research led by the University of Cincinnati Cancer Center's Trisha Wise-Draper showing a combination of immunotherapy medications can activate a robust immune response and help overcome treatment resistance in patients with refractory melanoma.
